Client/Family:
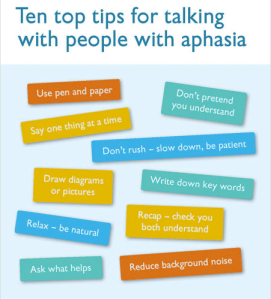
http://www.aphasia.org/content/communication-tips
- This webpage has a long list of dos and don’ts for caregivers about how to communicate with their loved one with aphasia. It provides useful tips to help communication partners re-establish their interactions, especially after their typically communication patterns have been abruptly altered. Many of these strategies are also beneficial for communication in general.
http://strokesupport.com/info/aphasia/aphasia_resources.htm
- This is another great resource for caregivers for those who have aphasia. It emphasizes self-care for the caregiver and provides coping mechanisms for dealing with the stresses and frustrations of communicating with someone who has aphasia. It gives suggestions for getting involved in their loved one’s therapy in the hospital and at home.
https://www.aphasia.com/about-aphasia/resources/
- This website provides a comprehensive list of website links which give tons of general information about what aphasia is, how it is assessed, how it can be treated, what the prognosis might look like, where to find help, and much more. The information found within the links on this page is endless and extremely useful for a person who has recently suffered a stroke and who has been diagnosed with aphasia.
SLP:
http://www.asha.org/Practice-Portal/Clinical-Topics/Aphasia/
- This website from ASHA has lots of information about aphasia for a speech-language pathologist who may not be familiar with what it is or how it is assessed or treated. This page has general information about the common practices of speech pathologists regarding aphasia. This could also be used as a way to explain aphasia to clients in terms that are easier to understand by non-speech/language professionals.
http://www.mnsu.edu/comdis/kuster2/sptherapy.html#aphasia
- This webpage has a large list of links for everything aphasia. From assessment tools to treatment techniques, this site has many options for treating all kinds of aphasic symptoms and deficits. This would be a good place to start if an SLP were unsure which approach for therapy to take.
http://www.aphasia.org/content/aphasia-therapy-guide
- This therapy guide for aphasia outlines two different approaches to aphasia therapy: the impairment approach and the communication approach. The impairment approach focuses on remediating deficits while the communication approach focuses on using the client’s strengths to compensate for their weaknesses. It is important to consider your client’s wants and needs when deciding what approach to take in therapy, as you want the approach to fit the client’s lifestyle and level of functioning.